Back and neck pain are some of the most common health complaints worldwide. For many people, this discomfort comes and goes and is often caused by muscle strain, poor posture, or long hours at work. But sometimes, persistent pain is not just “simple backache.” It may be a warning sign of a more serious condition — nerve compression in the spine.
Nerves are the body’s communication system. They carry signals from the brain to the muscles and organs, and vice versa. When nerves in the spine get compressed by a herniated disc, bone spur, thickened ligament, or other spinal changes, the signals are disrupted. This can cause pain, weakness, numbness, and, in severe cases, loss of important body functions.
Recognizing the early warning signs of nerve compression is essential to prevent permanent nerve damage. In this blog, we will explore what nerve compression is, why it happens, the symptoms you should never ignore, and when to seek help from a spine specialist.
What is Nerve Compression in the Spine?
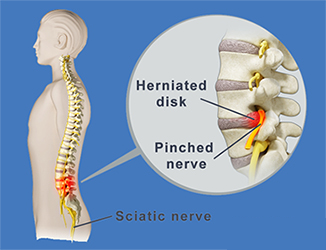
The human spine is made up of 33 vertebrae stacked on top of each other, cushioned by intervertebral discs. Spinal nerves exit the spinal cord through openings between these vertebrae.
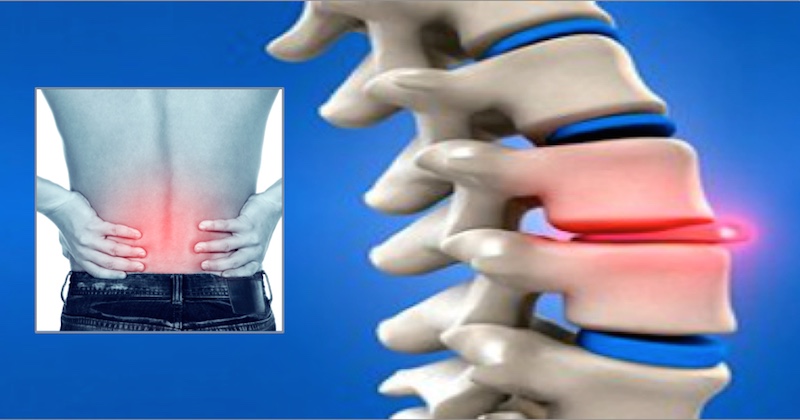
When a spinal disc bulges (herniated disc), bones develop spurs (osteophytes), or ligaments thicken due to aging or injury, they can press on the nearby nerves. This pressure is known as nerve compression or nerve impingement.
Nerve compression can occur at different levels of the spine:
Cervical spine (neck): Can affect shoulders, arms, and hands.
Thoracic spine (mid-back): Less common but may affect chest or abdomen.
Lumbar spine (lower back): Often causes sciatica, pain radiating into the legs.
Causes of Nerve Compression
Several conditions can lead to compression of spinal nerves:
Herniated or Bulging Disc – When the soft center of a disc pushes through its outer layer and presses on a nerve.
Degenerative Disc Disease – Age-related wear and tear that narrows space for nerves.
Spinal Stenosis – Narrowing of the spinal canal due to aging or arthritis.
Bone Spurs (Osteophytes) – Extra bone growth pressing on nerves.
Spinal Injury – Trauma, accidents, or falls can cause swelling or fracture that compresses nerves.
Tumors or Infections – Rare but possible causes.
Warning Signs of Nerve Compression
Early recognition of symptoms is critical. Here are the major warning signs you should never ignore:
1. Persistent Back or Neck Pain
Most muscle-related pain improves with rest, gentle exercise, or medication. But if the pain lasts for weeks or keeps returning, it may indicate something more serious.
2. Radiating Pain
Pain that travels along the nerve’s pathway is a hallmark sign of nerve compression.
Cervical compression → Pain spreading from neck to shoulders, arms, or fingers.
Lumbar compression → Pain traveling from lower back to buttocks, thighs, calves, or feet (sciatica).
This “shooting” or “electric shock-like” pain is different from dull muscular pain.
3. Numbness and Tingling
If you feel pins and needles, burning, or numbness in your arms, hands, legs, or feet, it suggests nerve irritation. This sensation is medically known as paresthesia.
4. Muscle Weakness
Compressed nerves cannot send proper signals to muscles. Over time, this may cause:
Weak grip strength.
Difficulty lifting objects.
Dropping things accidentally.
Trouble walking or climbing stairs.
Foot drop (inability to lift the front of the foot).
5. Balance and Coordination Problems
Nerve compression affects both strength and sensation, leading to unsteady walking, frequent stumbling, or poor coordination.
6. Loss of Reflexes
During clinical examination, doctors may notice reduced reflexes in elbows, knees, or ankles, pointing to nerve involvement.
7. Bladder or Bowel Dysfunction (Red Flag Symptom)
Sudden inability to control urination or bowel movements is a sign of severe nerve compression, often due to cauda equina syndrome. This is a medical emergency that needs immediate surgery to prevent permanent damage.
Risk Factors
Certain people are more likely to develop spinal nerve compression:
Age above 40 (degenerative changes).
Sedentary lifestyle and poor posture.
Obesity (extra load on spine).
Jobs requiring heavy lifting or long sitting hours.
Sports injuries or accidents.
Family history of spine disorders.
When to See a Doctor?
You should consult a spine specialist if:
Pain persists for more than 2–3 weeks.
Pain radiates to arms or legs.
You experience numbness, tingling, or weakness.
Walking and daily activities become difficult.
Sudden bladder or bowel control is lost (emergency).
Early consultation allows for accurate diagnosis through physical exam, X-rays, or MRI scans.
Diagnosis
A spine specialist may recommend:
Physical Examination – Checking pain areas, muscle strength, reflexes, and range of motion.
Imaging Tests – MRI, CT scan, or X-rays to visualize discs and nerves.
Nerve Studies – Electromyography (EMG) to assess nerve function.
Treatment Options
Treatment depends on the severity and underlying cause of compression.
Non-Surgical Management
Medications: Pain relievers, anti-inflammatory drugs, and muscle relaxants.
Physiotherapy: Exercises to strengthen spine-supporting muscles, improve flexibility, and correct posture.
Lifestyle Changes: Weight loss, ergonomic modifications at work, avoiding heavy lifting.
Injections: Corticosteroid or nerve block injections to reduce inflammation and pain.
Surgical Options
If non-surgical methods fail or symptoms worsen:
Microdiscectomy: Removal of herniated disc portion pressing on nerve.
Laminectomy: Removing part of vertebra to widen spinal canal.
Spinal Fusion: Stabilizing vertebrae for severe degeneration.
Endoscopic or Minimally Invasive Spine Surgery: Faster recovery, less pain.
Living with Nerve Compression
Many patients improve significantly with early treatment. However, untreated compression can cause permanent nerve damage leading to chronic pain, disability, or paralysis.
To protect your spine:
Maintain good posture while sitting and standing.
Exercise regularly, focusing on core and back strength.
Use ergonomic chairs and supportive mattresses.
Avoid smoking — it weakens spinal discs.
Maintain a healthy body weight.
Conclusion
Your spine is the backbone of your body — literally and figuratively. While occasional back or neck pain may be harmless, certain symptoms signal a deeper problem. Persistent pain, radiating pain, numbness, tingling, weakness, balance issues, and bladder/bowel changes are warning signs of nerve compression.
Ignoring these red flags can lead to irreversible nerve damage. But with early diagnosis and the right treatment, most patients recover well and return to their normal lives.
If you or a loved one notice these warning signs, don’t delay. Consult a qualified spine specialist. Acting early is the key to protecting your nerves, relieving pain, and ensuring a healthy, active life.