Back pain is one of the most common reasons people visit doctors, but not all back pain is the
same. While it’s often caused by muscle strain or poor posture, sometimes it signals a more
serious condition — such as a slipped disc (also called a herniated or prolapsed disc).
A slipped disc can cause a range of symptoms, from mild discomfort to severe pain and
weakness. The tricky part? Many people mistake the signs for simple muscle strain, delaying
treatment and risking complications.
In this article, we’ll cover:
● What a slipped disc is
● Why it happens
● Common signs and symptoms
● When to see a spine specialist
● Treatment options
● Prevention tips
What Is a Slipped Disc?
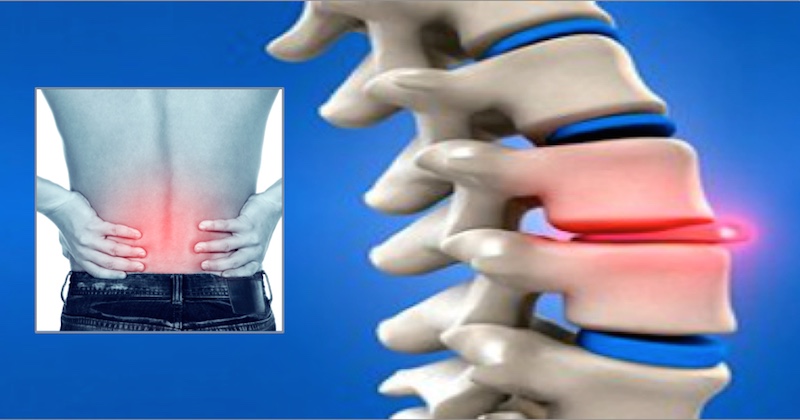
Your spine is a strong yet flexible structure made up of 33 vertebrae, separated by soft
cushions called intervertebral discs. These discs act like shock absorbers, protecting your
bones and nerves during movement.
Each disc has two parts:
● Nucleus pulposus – the jelly-like center
● Annulus fibrosus – the tough, rubbery outer ring
A slipped disc happens when the outer layer weakens or tears, allowing the soft inner material
to bulge or leak out. If it presses on a nearby nerve, it can cause pain, numbness, or weakness.
Slipped discs can occur anywhere along the spine, but they’re most common in the:
● Lumbar spine (lower back) – 90% of cases
● Cervical spine (neck) – less common but still significant
Why Does a Slipped Disc Happen?
Several factors can contribute to a slipped disc:
1. Aging – Discs lose water and flexibility over time, making them prone to tears.
2. Poor posture – Slouching or prolonged sitting increases spinal pressure.
3. Heavy lifting – Lifting with your back instead of your legs can cause sudden injury.
4. Repetitive strain – Jobs or sports with frequent bending, twisting, or lifting.
5. Excess weight – Extra body weight adds stress to the lower back.
6. Injury or trauma – Falls, accidents, or sports injuries can trigger disc damage.
Signs You Might Have a Slipped Disc
While only imaging tests like MRI can confirm a slipped disc, the following signs should not be
ignored.
1. Persistent Back or Neck Pain
● Lower back (lumbar herniation): Pain may worsen when bending, sitting, or lifting.
● Neck (cervical herniation): Pain may increase when turning the head or looking down.
Why it happens:
The damaged disc irritates surrounding nerves and muscles, causing inflammation and pain.
When to worry:
If pain lasts more than two weeks despite rest and basic care, it’s time to seek medical advice.
2. Radiating Pain (Arm or Leg)
If the herniated disc presses on a nerve, pain can travel along that nerve’s path.
● Sciatica: Pain radiates from the lower back into the buttocks, thighs, and calves.
● Cervical radiculopathy: Pain moves from the neck to the shoulders, arms, and even
fingers.
How it feels:
A sharp, burning, or electric shock-like sensation, often on one side of the body.
3. Numbness or Tingling
Nerve compression can disrupt normal sensation.
● Tingling (“pins and needles”) in arms, legs, hands, or feet
● Areas of reduced skin sensitivity
Warning:
If numbness spreads or worsens, it may indicate ongoing nerve damage.
4. Muscle Weakness
When nerve signals are blocked, muscles lose strength.
● Trouble lifting objects
● Difficulty gripping items
● Limping or dragging a foot
● Struggling with stairs
Why it matters:
Weakness means the nerve is significantly affected — a red flag that needs urgent attention.
5. Pain That Worsens With Movement
Certain actions can aggravate the pressure on the disc:
● Coughing or sneezing
● Twisting the spine
● Sitting for prolonged periods
If pain consistently spikes during these movements, it’s a sign the disc may be pressing on a
nerve.
6. Loss of Bladder or Bowel Control (Rare but Serious)
Known as Cauda Equina Syndrome, this is a medical emergency.
Symptoms include:
● Inability to control urination or bowel movements
● Severe numbness in the inner thighs or around the buttocks
● Intense back pain
If you notice these symptoms, seek emergency care immediately.
When to See a Spine Specialist
Not every case of back pain means you have a slipped disc, but you should see a specialist if
you have:
● Pain lasting more than 2–3 weeks
● Pain radiating into arms or legs
● Numbness, tingling, or weakness
● Severe pain after injury
● Difficulty walking or moving normally
● Loss of bladder or bowel control
Why early consultation matters:
● Prevents further nerve damage
● Increases the chances of recovery without surgery
● Reduces the risk of chronic pain
How a Spine Specialist Diagnoses a Slipped Disc
A specialist will:
1. Take a detailed medical history
2. Perform a physical and neurological examination
3. Recommend imaging tests such as:
○ MRI (most accurate)
○ CT Scan
○ X-rays (to rule out other conditions)
Treatment Options for a Slipped Disc
Non-Surgical Treatments
Most cases improve with conservative methods:
1. Medications – Pain relievers, anti-inflammatories, muscle relaxants.
2. Physiotherapy – Targeted exercises to strengthen the spine and core.
3. Lifestyle changes – Weight management, ergonomic improvements.
4. Epidural steroid injections – Reduce inflammation around the nerve.
Surgical Treatments
If symptoms don’t improve after several weeks or worsen, surgery may be considered.
● Microdiscectomy: Removing part of the disc to relieve pressure.
● Endoscopic discectomy: Minimally invasive approach.
● Spinal fusion: In severe cases with instability.
Recovery and Prognosis
With proper treatment, most people recover fully from a slipped disc within a few weeks to a few
months. Factors affecting recovery include:
● Severity of nerve compression
● Age and general health
● How quickly treatment was started
How to Prevent a Slipped Disc
While some causes (like aging) can’t be avoided, you can reduce your risk by:
● Maintaining a healthy weight
● Exercising regularly to strengthen core muscles
● Practicing good posture
● Using correct lifting techniques
● Avoiding smoking, which weakens spinal discs
Final Thoughts
A slipped disc may sound alarming, but with early diagnosis and the right treatment, most
patients recover well without surgery. The key is to listen to your body — persistent pain,
numbness, or weakness is not something to ignore.
If you suspect you have a slipped disc, consult a qualified spine specialist. Early care not only
relieves symptoms faster but also prevents long-term complications.
Remember: Your spine is central to your movement and quality of life — treat it with the care it
deserves.