Back pain is one of the most common health complaints worldwide, and among its
many causes, a herniated disc is one of the most frequent — and often misunderstood
— conditions.
If you’ve been told you have a herniated disc or suspect you might, understanding what
it is, why it happens, and how it can be treated is the first step toward recovery.
1. What Is a Herniated Disc?
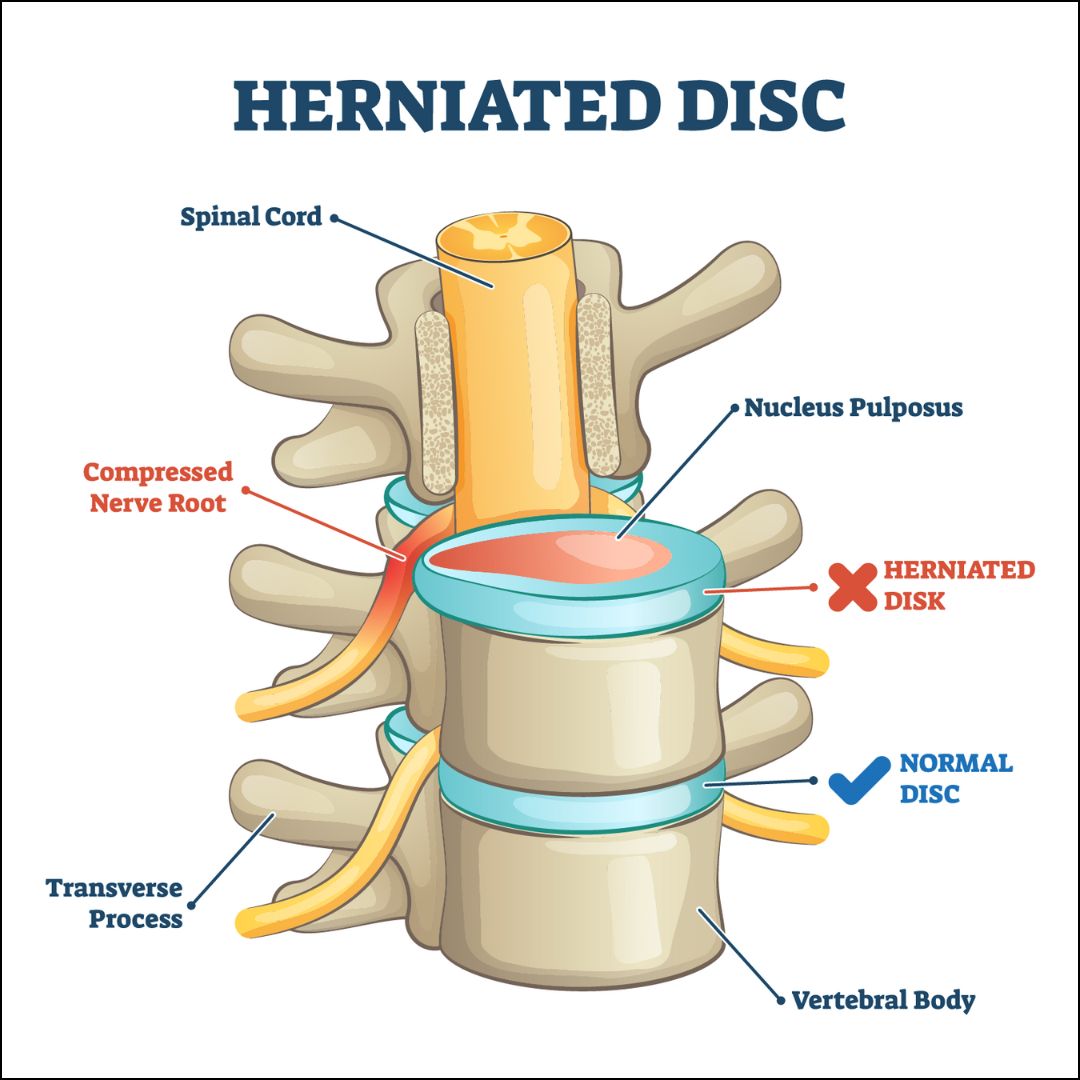
Your spine is made up of vertebrae (bones) stacked one on top of another, separated
by soft, cushion-like structures called intervertebral discs. These discs act like shock
absorbers, protecting the spine from wear and tear during movement.
Each disc has two main parts:
● Nucleus Pulposus – the soft, gel-like center.
● Annulus Fibrosus – the tough, fibrous outer ring.
A herniated disc (also called a slipped disc, ruptured disc, or disc prolapse) occurs
when a tear in the annulus allows part of the nucleus to push out. This can press on
nearby nerves, causing pain, numbness, or weakness.
2. How Common Is It?
Herniated discs are more common than most people think:
● Most often occur in people aged 30 to 50 years.
● Men are slightly more affected than women.
● Can occur in the neck (cervical spine) or lower back (lumbar spine), but the
lumbar region is the most common site.
3. Causes of Herniated Disc
A herniated disc doesn’t usually happen overnight — it’s often the result of gradual
wear and tear. Common causes include:
a) Age-Related Degeneration
Over time, spinal discs lose water content, making them less flexible and more prone to
tearing.
b) Repetitive Strain
Jobs or activities involving heavy lifting, bending, or twisting can increase the risk.
c) Injury or Trauma
Sudden impact from falls, accidents, or sports injuries can cause a disc to rupture.
d) Poor Posture & Sedentary Lifestyle
Sitting for long periods, especially with poor ergonomics, puts stress on the spine.
e) Genetic Factors
Some people inherit a tendency toward disc problems.
f) Obesity
Extra weight increases pressure on spinal discs.
4. Symptoms of a Herniated Disc
Symptoms depend on the disc’s location and whether it is pressing on a nerve.
a) Lumbar (Lower Back) Herniated Disc
● Sharp or burning pain radiating down the leg (sciatica)
● Numbness or tingling in leg or foot
● Muscle weakness in lower extremities
● Pain worsens with sitting, bending, or lifting
b) Cervical (Neck) Herniated Disc
● Pain in neck, shoulder, arm, or hand
● Numbness or tingling in arm or fingers
● Weakness in arm muscles
● Reduced range of motion in neck
c) Red Flag Symptoms – Seek Immediate Medical Help
● Loss of bladder or bowel control (cauda equina syndrome)
● Severe weakness or paralysis
● Intense, unrelenting pain
5. How Is a Herniated Disc Diagnosed?
Your doctor will start with a detailed medical history and physical examination,
checking for muscle strength, reflexes, and sensation.
Diagnostic tests may include:
● MRI Scan – Best for visualizing soft tissues like discs and nerves.
● CT Scan – Useful if MRI isn’t possible.
● X-rays – To rule out fractures or bone issues.
● Nerve Conduction Studies / EMG – Assess nerve function.
6. Treatment Options for Herniated Disc
Not all herniated discs require surgery — in fact, most improve with non-surgical
treatment.
A) Conservative (Non-Surgical) Management
1. Rest & Activity Modification – Avoid heavy lifting or movements that worsen
symptoms.
2. Medications –
○ Pain relievers (paracetamol, NSAIDs)
○ Muscle relaxants
○ Nerve pain medications (gabapentin, pregabalin)
3. Physiotherapy – Exercises to strengthen core muscles, improve flexibility, and
reduce pressure on the disc.
4. Hot or Cold Therapy – Helps reduce inflammation and muscle spasm.
5. Epidural Steroid Injections – For severe inflammation and nerve pain.
Tip: Staying active within limits is better than prolonged bed rest.
B) Surgical Options
Surgery is considered if:
● Symptoms persist beyond 6–12 weeks of conservative care.
● There is severe weakness or nerve damage.
● Bowel or bladder dysfunction occurs.
Common surgical procedures include:
1. Microdiscectomy – Removing the herniated portion through a small incision
using magnification tools.
2. Endoscopic Discectomy – Minimally invasive procedure using a small camera
for precision.
3. Laminectomy – Removing part of the bone to relieve nerve pressure.
Advantages of Minimally Invasive Surgery:
● Smaller incision
● Less muscle damage
● Faster recovery
● Shorter hospital stay
7. Recovery & Rehabilitation
Whether you have surgery or not, rehabilitation is key:
● Physiotherapy – To restore strength, posture, and flexibility.
● Ergonomic Adjustments – Correct chair height, computer position, and
sleeping posture.
● Gradual Return to Activities – Avoid sudden heavy lifting for several weeks.
8. Preventing a Herniated Disc
While not all cases can be prevented, you can lower your risk with:
● Regular Exercise – Strengthen core muscles to support the spine.
● Healthy Weight – Reduce strain on the spine.
● Good Posture – Keep spine aligned while sitting, standing, and lifting.
● Safe Lifting Techniques – Bend knees, not waist.
● Quit Smoking – Nicotine accelerates disc degeneration.
9. Living with a Herniated Disc
Many people live active, pain-free lives after a herniated disc diagnosis — especially
with early intervention. The key is to listen to your body, follow medical advice, and
stay consistent with rehabilitation exercises.
Final Thoughts
A herniated disc can sound alarming, but it’s a treatable condition. With timely
diagnosis, proper treatment, and lifestyle changes, you can recover and get back to
normal life. If you experience severe back or neck pain, especially with numbness,
tingling, or weakness, consult a spine specialist promptly.